- VT = Ventricular tachycardia
- Afib = Atrial fibrillation
- AVRT = Atrioventricular reentry tachy
- AVNRT= Nodal AVRT
- RBBB = Right bundle branch block
- LBBB = Left bundle branch block
- WPW = Wolff-Parkinson-White syndrome
EKG practice test
14 April,2015 Antoine AyerQuiz-summary
0 of 30 questions completed
Questions:
- 1
- 2
- 3
- 4
- 5
- 6
- 7
- 8
- 9
- 10
- 11
- 12
- 13
- 14
- 15
- 16
- 17
- 18
- 19
- 20
- 21
- 22
- 23
- 24
- 25
- 26
- 27
- 28
- 29
- 30
Information
This quiz contains several brief medical histories and their matching ECGs. For each question, you should check between 0 to 4 diagnoses. If the blood pressure is not specified, it means that it is in the normal range.
Remember: Do not use your browser’s “back” button. The result is shown only when you have answered every question.
Enjoy!
You have already completed the quiz before. Hence you can not start it again.
Quiz is loading...
You must sign in or sign up to start the quiz.
You have to finish following quiz, to start this quiz:
Results
0 of 30 questions answered correctly
Your time:
Time has elapsed
You have reached 0 of 0 points, (0)
| Average score |
|
| Your score |
|
Categories
- Not categorized 0%
-
You should improve your ECG skills to optimize your decisions regarding patient triage. You can find interesting educative resources in our link section.
You are welcome to retake the quiz “EKG practice test” or try another Quiz.
-
Congratulations! You passed “EKG practice test” quiz.
| Pos. | Name | Entered on | Points | Result |
|---|---|---|---|---|
| Table is loading | ||||
| No data available | ||||
- 1
- 2
- 3
- 4
- 5
- 6
- 7
- 8
- 9
- 10
- 11
- 12
- 13
- 14
- 15
- 16
- 17
- 18
- 19
- 20
- 21
- 22
- 23
- 24
- 25
- 26
- 27
- 28
- 29
- 30
- Answered
- Review
-
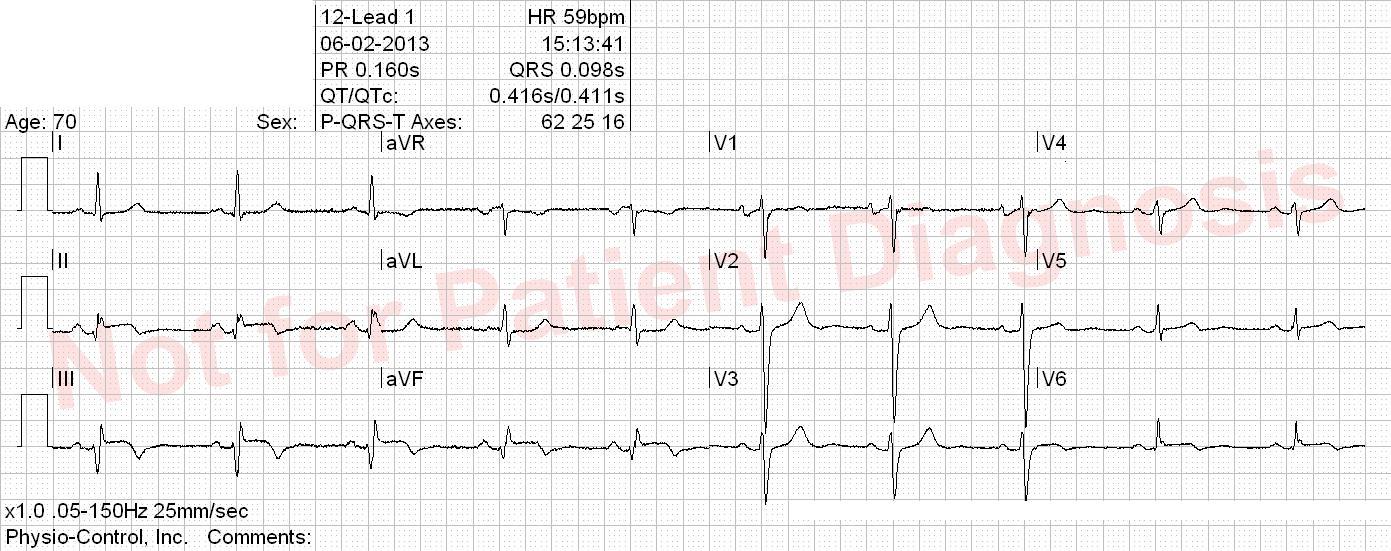
Question 1 of 30
1. Question
Woke up with central oppressive chest pain which are increase with deep inspiration and when lying on the back.
Correct
Incorrect
-
Question 2 of 30
2. Question
Correct
Incorrect
-
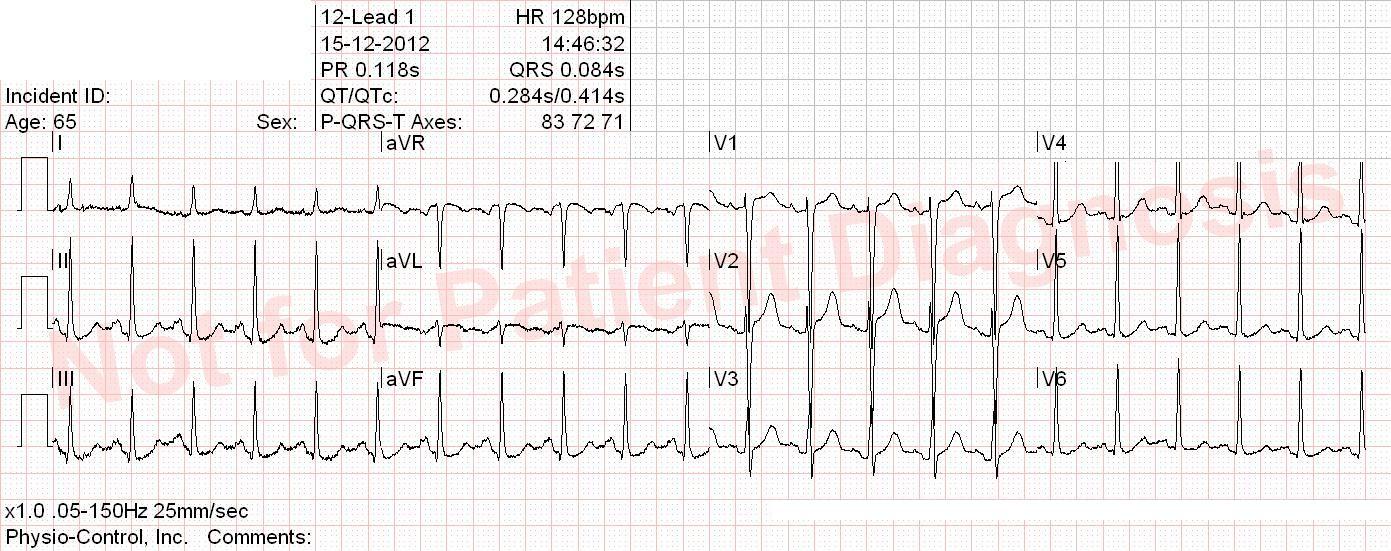
Question 3 of 30
3. Question
Oppressive left lateral chest pain for 5 hours and impression sleeping left arm. BP 177/95 mmHg. Nitroglycerin spray has some effect on the pain.
Correct
Incorrect
-
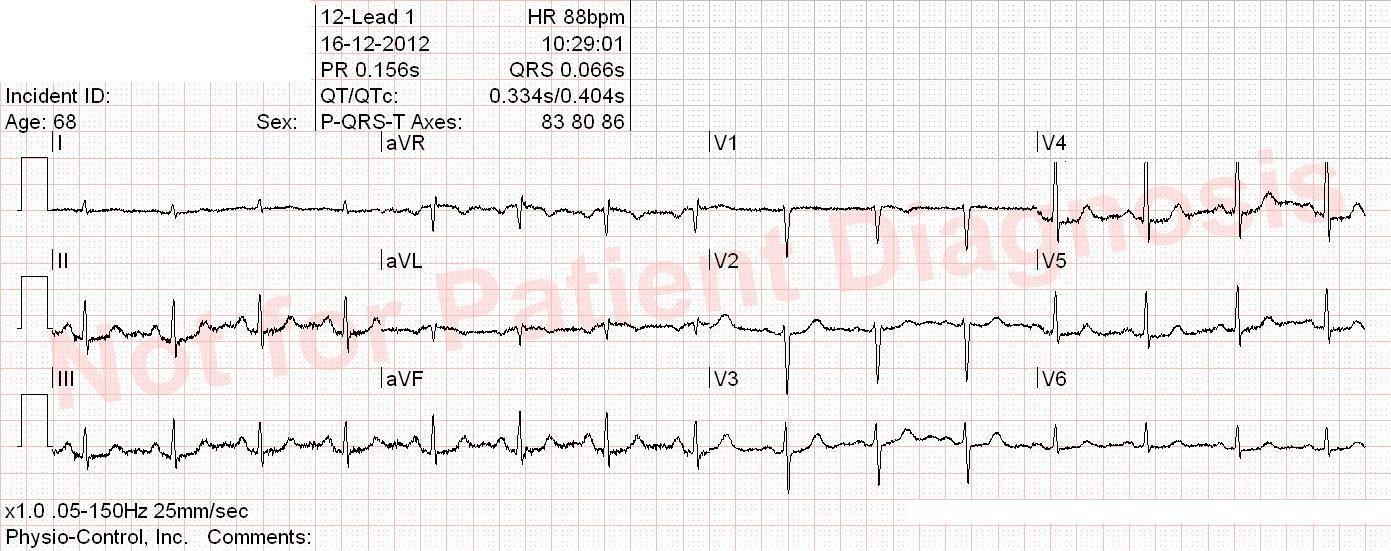
Question 4 of 30
4. Question
This patient has diabetes, has an history of previous myocardial infarction and complains of dyspnea and chills. Temperature 39°C
Correct
Incorrect
-
Question 5 of 30
5. Question
Correct
The difference between atrial fibrillation (A-fib) and atrial flutter (A-flutter), is clinically relevant because typical flutter can easily be treated by radiofrequency ablation. A-fib and atypical A-flutter requires more expertise and radiofrequency ablation has lower success rate.
Atrial flutter:
Atrial rate ca. 300 bpm (200-400 bpm) with a heart rate typically ca. 150 bpm.
- Typical (type I) atrial flutter: saw-tooth-like waves
- Counterclockwise: negative flutter waves in II, III, aVF and positive in V1
- Clockwise: positive flutter waves in II, III, aVF and negative in V1
- Atypical (type II) atrial flutter: doesn
Incorrect
The difference between atrial fibrillation (A-fib) and atrial flutter (A-flutter), is clinically relevant because typical flutter can easily be treated by radiofrequency ablation. A-fib and atypical A-flutter requires more expertise and radiofrequency ablation has lower success rate.
Atrial flutter:
Atrial rate ca. 300 bpm (200-400 bpm) with a heart rate typically ca. 150 bpm.
- Typical (type I) atrial flutter: saw-tooth-like waves
- Counterclockwise: negative flutter waves in II, III, aVF and positive in V1
- Clockwise: positive flutter waves in II, III, aVF and negative in V1
- Atypical (type II) atrial flutter: doesn
- Typical (type I) atrial flutter: saw-tooth-like waves
-
Question 6 of 30
6. Question
Former smoker with hypertension. He woke up this morning with a tingling sensation in both arms. No chest pain. BP 210/93 mmHg. Symptoms disappear completely after nitro spray.
Correct
Incorrect
-
Question 7 of 30
7. Question
Smoker with hypertension and high cholesterol. Shortness of breath over the last few weeks, recurrent stabbing retrosternal chest pain.
Correct
Incorrect
-
Question 8 of 30
8. Question
Correct
Incorrect
-
Question 9 of 30
9. Question
Correct
Incorrect
-
Question 10 of 30
10. Question
Correct
Incorrect
-
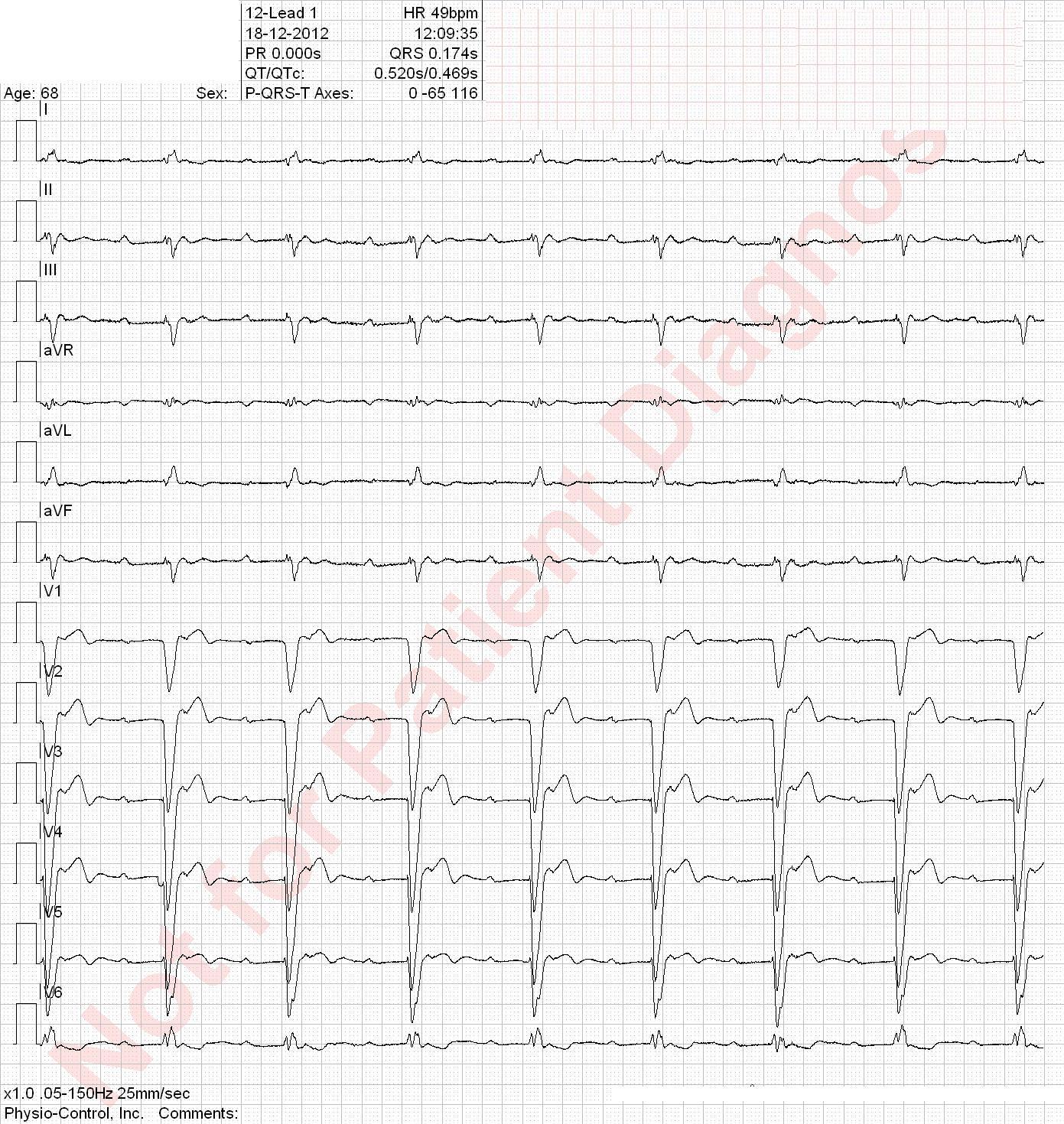
Question 11 of 30
11. Question
Active smoker. After this patient woke up, suddent onset of severe chest pain on the left lateral region of the chest and between the shoulder blades.
Correct
Anterior STEMI! This patient’s LAD was occluded. Inferior Q waves are not significant.
Incorrect
Anterior STEMI! This patient’s LAD was occluded. Inferior Q waves are not significant.
-
Question 12 of 30
12. Question
Young patient with one hour of palpitation, mild chest oppression and discrete shortness of breath and dizziness. Has had several similar episodes among the last few years.
Correct
Incorrect
-
Question 13 of 30
13. Question
Smoker. Two episodes with typical chest pain. The patient goes to his GP and receives nitroglycerin spray with some effect.
Correct
Incorrect
-
Question 14 of 30
14. Question
Previously healthy woman with a presyncope. Had a “unquiet heart” over the last 50 years but has never been properly investigated.
Correct
Incorrect
-
Question 15 of 30
15. Question
Correct
Incorrect
-
Question 16 of 30
16. Question
Known with diabetes, ischemic heart disease and COPD. Increasing shortness of breath. Known with daily intermittent chest pain.
Correct
Incorrect
-
Question 17 of 30
17. Question
CABG 15 years ago. Transcatheter aortic valve implantation 1 month ago. Severe chest pain and shortness of breath for one hour, palor and cold sweats. BP 160/90 mmHg.
Correct
Incorrect
-
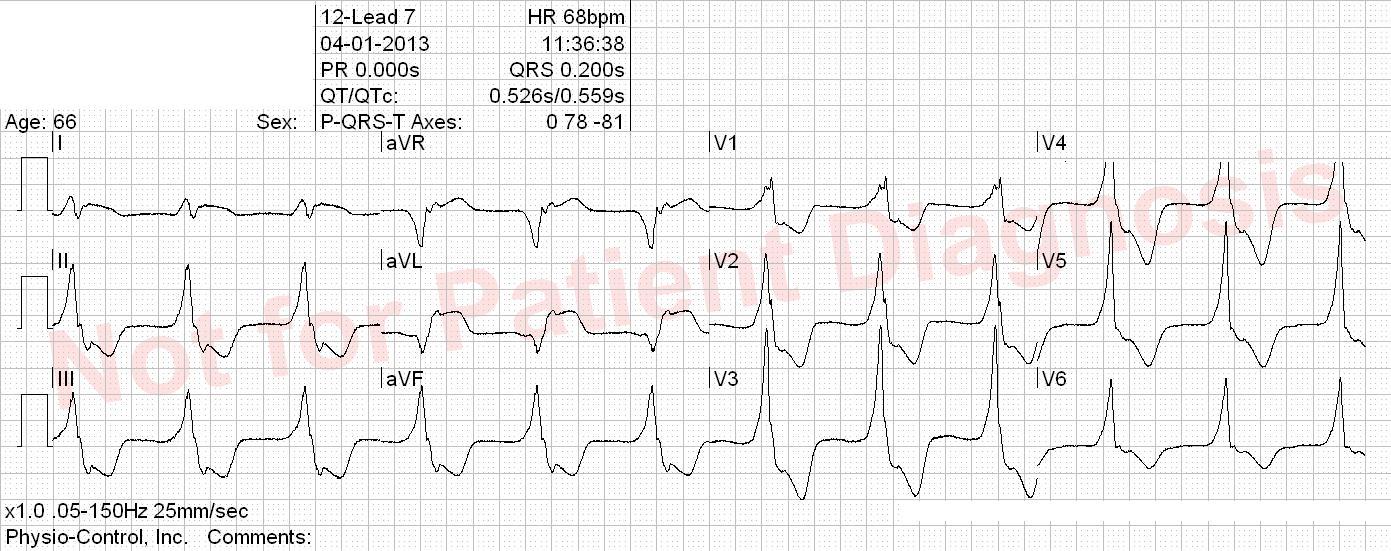
Question 18 of 30
18. Question
Previously healthy. 1 ½ hours with strong, oppressive retorsternal chest pain and dyspnea. Good effect of nitroglycerin given prehospitaly. Pale and clammy skin. Has usually a normal ECG.
Correct
Incorrect
-
Question 19 of 30
19. Question
Correct
Incorrect
-
Question 20 of 30
20. Question
Correct
Incorrect
-
Question 21 of 30
21. Question
History of prior CABG. Known with left bundle branch block. 3 days with shortness of breath, cough and fever. Normal BP.
Correct
Incorrect
-
Question 22 of 30
22. Question
Previously healthy patient. Chest pain for several days radiating to the neck and left arm. Distinct worsening for 30 minutes.
Correct
Incorrect
-
Question 23 of 30
23. Question
Former smoker with hypertension and atrial fibrillation. Cardiac arrest with VF. CPR 3 minutes. Defibrillated to this ECG.
Correct
Incorrect
-
Question 24 of 30
24. Question
Former smoker patient with a family history of cardiovascular disease. Over the last few days, he had intermittent pricking sensation in the chest. Marked deterioration one hour ago with the pain radiating now to the neck.
Correct
Incorrect
-
Question 25 of 30
25. Question
This patient had nausea when he woke up this morning but he has now severe chest pain which started an hour ago.
Correct
Incorrect
-
Question 26 of 30
26. Question
Correct
Incorrect
-
Question 27 of 30
27. Question
CABG in 2003. Chest pain since yesterday. The pain is aggravating after he had been working with a showel in the snow.
Correct
Incorrect
-
Question 28 of 30
28. Question
Correct
There is diffuse concave non-significant ST elevation which could indicate pericarditis.
Incorrect
There is diffuse concave non-significant ST elevation which could indicate pericarditis.
-
Question 29 of 30
29. Question
Known with ischemic heart disease, atrial fibrillation and pacemaker. This afternoon onset of malaise, coughing, chest pain localized in the left side and neck pain. A bit of dyspnea as well.
Correct
Incorrect
-
Question 30 of 30
30. Question
Known to have hypertension and being a former smoker. Acute onset of oppressive chest pain that radiates to his jaw.
Correct
Incorrect